
It might seem reasonable that we should all be taking this supplement. But hold on. The argument for taking Vitamin D assumes a few things. First, that low Vitamin D actually causes all of the conditions it is associated with. This is not necessarily true. Low Vitamin D could cause (or contribute to) heart disease, but it could also be that heart disease causes low Vitamin D. Another possibility is that some third factor causes both low Vitamin D and heart disease.
Even if we can prove some causation, we then need to assume that correcting the Vitamin D deficiency will prevent the disease. This may not be true either. Low Vitamin D may be an indicator of overall poor health, which increases the risk for cardiac disease. It could appear that low Vitamin D contributes to the condition. But raising the Vitamin D will not help because it will just fix the symptom, not the underlying problem.
Fortunately we have studies that can help figure this out. Currently the best way to answer a question of clinical relevance is with a large, well-executed randomized controlled trial (RCT). An RCT works like this: enroll the participants you want to study and randomly assign half of them to receive a treatment and the other half to receive a placebo. Those receiving the treatment are called the intervention group. The other group is the control group. Ideally, the two groups will be similar in every way except the treatment – they will have the same distribution in age, income, race, gender, and health status. They will even receive pills that look identical, though half will be placebos. If, at the end of the study, there are differences between the two groups, we can attribute those differences to the treatment.
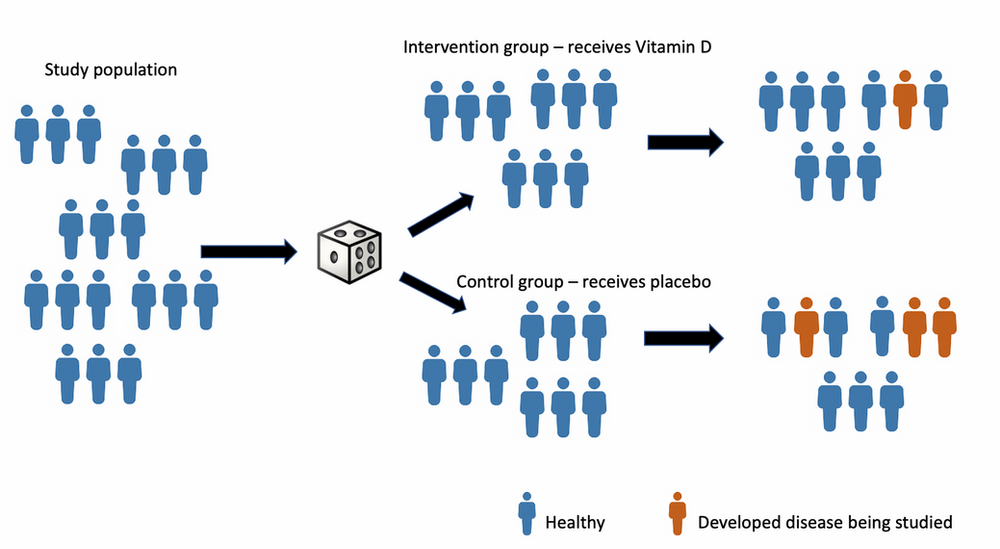
RCTs are costly and time intensive, so generally we will only be able to study the interventions and outcomes that have the highest chance of showing a benefit. We base this on prior studies; if several large observational studies show a correlation between Vitamin D and heart disease, then this is something we should study with an RCT.
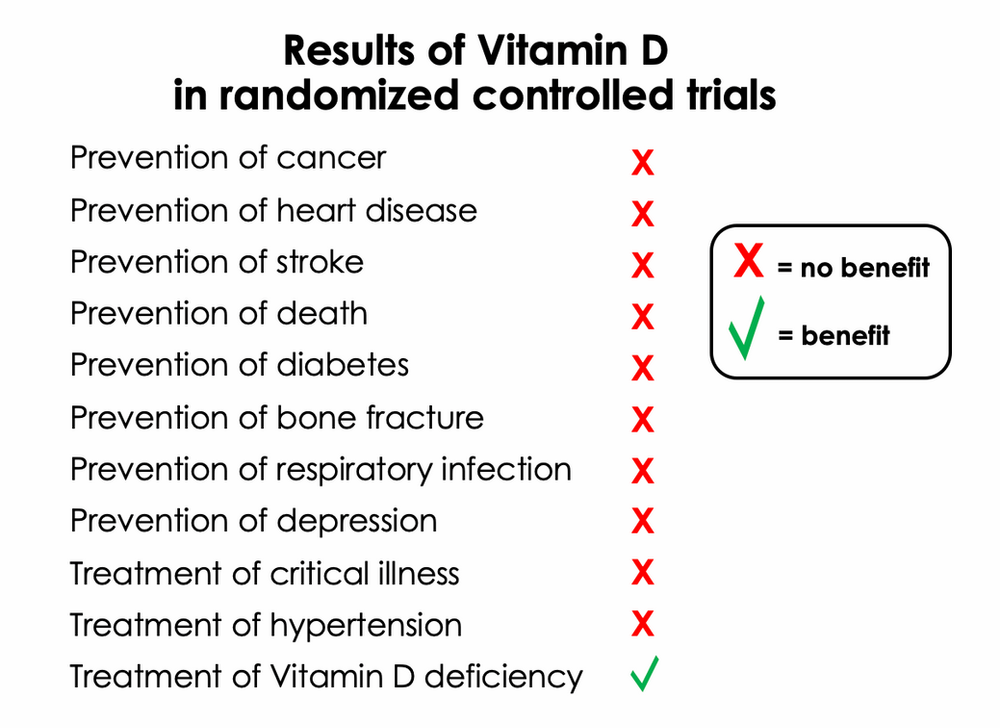
We now have results for over 1500 RCTs on Vitamin D supplementation. Some of the largest and most significant trials are listed and summarized at the end of this article. When tested on its ability to prevent disease, Vitamin D has failed to live up to expectations.
One of the largest and best studies we have is called VITAL, led by Dr. JoAnn Manson at Brigham and Women's Hospital in Boston. Over 25,000 adults (men age 50 and older, women age 55 and older) with no history of cardiovascular disease or cancer participated in the study. They received either 2,000 IUs of Vitamin D3 or placebo daily for five years. Researchers evaluated the rates of cancer and major cardiovascular events including stroke, heart attack, and cardiovascular death.
The result: Vitamin D failed to prevent cancer, stroke, heart attack, or cardiovascular death. These conditions occurred at the same rate in those receiving Vitamin D and those receiving placebo. There was one positive finding, though: in a post hoc analysis, it seemed that Vitamin D decreased the mortality from cancer when the initial two years were excluded. Post hoc (“after the event”) analyses can be quite useful, but need to be viewed with some skepticism. In high-quality RCTs (like VITAL), the outcome measures and statistical analyses are specified prior to data collection. Sometimes, as in VITAL’s case, an unexpected outcome may appear at the time the data are evaluated, prompting a post hoc analysis. In this case, when results from the first two years were excluded, the rate of cancer death was 1.2% in the placebo group, and 0.9% in the Vitamin D group - 25% reduction in cancer mortality, though the absolute numbers were low. It is not possible to draw too many conclusions from this, but it is something to note for future studies.
Even in studies of bone health, Vitamin D has been disappointing. We already know that Vitamin D is essential in calcium metabolism, and Vitamin D deficiency can lead to bone disorders like rickets and osteomalacia. Taking Vitamin D to treat severe Vitamin D deficiency is necessary for the treatment of these conditions. But in the large trials looking at Vitamin D's ability to prevent bone loss, the participants were taken from the general population, many of whom had normal Vitamin D levels. For severely deficient individuals (only a small percentage of the population), there are clear benefits to supplementation. These benefits do not appear to extend to those with normal levels or mild deficiencies.
Large randomized controlled trials are currently the best way to evaluate a treatment, but they are difficult to do. If done well, an RCT is expensive, time intensive, and challenging to coordinate. It is worth it if we can answer our question adequately, but sometimes we realize after the trial that we needed to account for something else, or that we need more people in the study before we can really answer our question. In addition, RCTs will not always give definitive answers. Sometimes two or more small trials of the same treatment will show opposite results, and we need to reconcile those. Simply redoing an RCT is usually not an option. Instead, scientists have developed a method of combining similar RCTs and analyzing them together, in what is called a meta-analysis.
Meta-analyses have exploded in popularity over the last few decades. If done well, a meta-analysis of a group of trials can reveal insights that cannot be seen in the individual trials. Unfortunately there are potential problems. The quality of the meta-analysis depends on the quality of the studies it includes, which can lead to erroneous results when poor quality studies are present (garbage in, garbage out).
In addition, publication bias may incorrectly amplify a treatment effect. Publication bias occurs when researchers decide to publish only “positive” findings – studies that show a treatment effect. Suppose ten small trials of Vitamin D are performed. Five show a benefit to Vitamin D and five do not. Researchers and journals are much more inclined to publish positive results than negative, so it is possible that only the five positive studies will make it into the medical literature. A meta-analysis on the five published positive studies will show a much stronger effect of Vitamin D than a meta-analysis that included all ten studies.

Where negative studies go to die.
Robert Rosenthal called publication bias "the file drawer problem" because important negative studies often end up here. Photo by nirat on bigstockphoto.com.
Not every related trial should be included in a meta-analysis, though. One of the major challenges in performing these analyses is deciding which studies to include or exclude. Ideally only high-quality, well-designed, well-executed studies will be included. Researchers do not always agree on which studies to include, and differences in inclusion criteria have led to similar meta-analyses producing opposite results. ,This has occurred in studies of Vitamin D and fracture risk in older adults, with some meta-analyses showing zero benefit to Vitamin D and others showing a decreased risk of fracture, even though they included many of the same studies.
In addition to being high quality, the included studies should all try to answer the same clinical question. Many meta-analyses can only be done by combining trials that differ in important details, like the age of participants, treatment dosages, or definition of endpoints. Combining these may be feasible, but the clinical relevance may change when disparate groups are lumped together. For example, suppose we want to know if Vitamin D prevents asthma attacks in children. If a meta-analysis shows a small benefit to Vitamin D when all ages are combined, but the individual small studies in children did not show a benefit, what do I advise a 10 year old with asthma?
Despite these challenges, meta-analyses of RCTs can provide meaningful insights. Unfortunately, most high-quality meta-analyses show similar results to our individual randomized controlled trials: Vitamin D does not appear to prevent disease in healthy adults.
But there are a few promising areas identified in meta-analyses. Note that some of these findings are not consistent with the large RCTs and will need to be studied further before definitive recommendations can be made.
The areas in which meta-analyses have identified benefits from Vitamin D:
All of these findings will require more research to quantify Vitamin D’s role – and further studies may disappoint.

You don't need this much Vitamin D.
Photo by Koldunov at bigstockphoto.com.
Given the hype surrounding Vitamin D, the lack of significant benefit for the general population in high-quality trials may seem surprising. How can we reconcile promising early observational studies linking Vitamin D to most major causes of death with our current results? One thing that seems increasingly clear is that in most cases low Vitamin D (truly low Vitamin D) is a marker of poor health rather than a cause. Vitamin D is made in the skin after exposure to sunlight. A chronically ill, frail individual may leave the house less often, leading to lower Vitamin D levels. Fixing the Vitamin D will not fix the chronic illness.
In some situations low Vitamin D does contribute to illness, but this is generally in cases of severe deficiency. We know that severe Vitamin D deficiency leads to bone disorders like rickets and osteomalacia. This provides a plausible scenario by which Vitamin D deficiency could increase mortality in the elderly: Without sunlight, a frail elderly woman may develop bone loss, increasing her risk of fractures. Fractures in the elderly have shockingly high mortality rates – so in this case a severe Vitamin D deficiency could contribute to death, and supplementation would help. For the majority of healthy adults, supplementation is unnecessary.
None of the studies reviewed are perfect. Any given study is going to have weaknesses - maybe the researchers ignored a factor that we now know to be important (but wasn't known when the trial was designed), or a lot of patients were lost to follow-up (very common when trying to follow people for many years), or the study was not large enough (something researchers are always thinking about). In many of the studies reviewed here, Vitamin D was given to a general population of older adults. They were not selected for Vitamin D deficiency. This was done on purpose to allow us to determine whether we should advise everyone to take Vitamin D supplements for disease prevention. If we only studied those with severe deficiency, we likely would have seen more benefits from supplementation. But we already have very good evidence that severe Vitamin D deficiency (i.e. under 10 ng/ml or 25 nmol/l) is detrimental and should be treated. Future studies will need to evaluate milder Vitamin D deficiencies to see if those levels require treatment.
1. Recognize that Vitamin D is not a panacea. It is an essential hormone, definitely, but not a magical pill that will ward off disease. There are conditions that benefit from Vitamin D supplementation - for hypoparathyroidism, a condition that can cause dangerously low calcium levels, Vitamin D is lifesaving. For otherwise healthy adults, the benefit is less clear.
2. Use a reasoned approach to supplementation. There are benefits to Vitamin D in cases of severe deficiency (not mild deficiency). If you are elderly, frail, and not getting sunlight, there is a chance you are significantly deficient in Vitamin D. If you think you may be deficient, you can check this with a blood test.
3. Act in moderation. Low to moderate doses of Vitamin D (e.g. 400 to 2000 IUs daily) have proven to be safe in trials. If you think there is a benefit and we just don't have enough data to prove it yet, you may be right. We do know the harms of taking too much, though, so supplement in moderation. And if you are taking Vitamin D, ask your doctor to check your blood levels.
Finally, no one needs to blindly believe what I say - or what anyone else says - about Vitamin D. You can and should critically evaluate the evidence for yourself. Below I have listed out some of the most important RCTs and meta-analyses of RCTs, with summaries and links. When looking at meta-analyses, Cochrane always provides top quality reviews, and I often look to them first for quality analyses and thoughtful interpretations.
A sample of the largest and best RCTs on Vitamin D, grouped by condition
VITAL trial (2018, U.S.)
Participants: 25,871 healthy adults over age 50, making it our largest trial
Intervention: 2,000 international units (IUs) of Vitamin D daily vs. placebo, for five years
Outcome measure: incidence of cancer or major cardiovascular event (heart attack, stroke, or death from cardiovascular causes)
Findings: No benefit
ViDA (Vitamin D Assessment) Trial (2017, New Zealand)
Participants: 5,108 adults ages 50 to 84
Intervention: 100,000 IUs of Vitamin D monthly vs. placebo for three years
Outcome measure: rate of cardiovascular disease, cancer, and non-vertebral fractures
Findings: No benefit
RECORD trial follow-up study (2012, United Kingdom)
Participants: 5,292 adults over age 70 with history of fracture
Intervention: 800 IUs Vitamin D daily vs. placebo for 24 to 62 months, with follow-up three years later
Outcome measure: cancer incidence, mortality
Findings: No benefit
EVITA (Effect of Vitamin D on Mortality in Heart Failure) (2017, Germany)
Participants: 400 Vitamin D-deficient adults with heart failure
Intervention: 4000 IUs Vitamin D3 daily for three years
Outcome measure: mortality
Findings: No benefit
RECORD Trial (2005, United Kingdom)
Participants: 5,292 adults over age 70 with history of fracture
Intervention: 800 IUs Vitamin D daily vs. placebo for 24 to 62 months
Outcome measure: new fractures
Findings: No benefit
Older women at risk for fracture (2018, Australia)
Participants: 2,256 women age 70 and older
Intervention: 500,000 IUs Vitamin D3 yearly vs. placebo for 3 to 5 years
Outcome measures: falls and fractures
Findings: Harm: high-dose Vitamin D increased falls and fractures, particularly in the first three months after receiving Vitamin D
VITAL-BONE Trial (2020, U.S.)
Participants: 771 adults over age 50 (VITAL study participants)
Intervention: 2000 international units (IUs) of Vitamin D daily vs. placebo, for five years
Outcome measure: change in bone mineral density, bone structure
Findings: No benefit
Vitamin D and calcium for patients on corticosteroids (1996, U.S.)
Participants: 96 adults with rheumatoid arthritis, 65 of them on corticosteroids
Intervention: 500 IUs daily of Vitamin D3 and 1000 mg daily of calcium for 2 years
Outcome measure: bone density
Findings: Benefit: Calcium and Vitamin D prevented corticosteroid-induced bone density
D2d Trial (2019, U.S.)
Participants: 2,423 adults at high risk for developing diabetes (they had pre-diabetes)
Intervention: 4,000 IUs of Vitamin D daily vs. placebo for 2.5 years
Outcome measure: development of diabetes
Findings: No benefit
DAYLIGHT Trial
Participants: 534 Vitamin-D deficient adults aged 18 to 50 with prehypertension or hypertension
Intervention: 4,000 IUs of Vitamin D3 daily vs. 400 IUs daily for 6 months
Outcome measure: reduction in blood pressure
Findings: No benefit
VIOLET (Vitamin D to Improve Outcomes by Leveraging Early Treatment) trial (2019, U.S.)
Participants: 1,078 critically ill, Vitamin D-deficient adults
Intervention: one dose of 540,000 IU of vitamin D3
Outcome measure: death after 90 days
Findings: No benefit
VITdAL ICU Trial (2014, Austria)
Participants: 492 critically ill, Vitamin D-deficient adults
Intervention: 540,000 IU Vitamin D3 once, then 90,000 IU monthly for 5 months
Outcome measure: hospital length of stay, mortality
Findings: No benefit
Children at risk for tuberculosis (2020, Mongolia)
Participants: 8,851 Vitamin D-deficient schoolchildren
Intervention: 14,000 IUs of Vitamin D3 weekly vs. placebo for 3 years
Outcome measure: tuberculosis infections and acute respiratory infections
Findings: No benefit
Children at risk for pneumonia (2012, Afghanistan)
Participants: 3,046 infants ages 1 to 11 months
Intervention: 100,000 IU Vitamin D every 3 months vs. placebo for 18 months
Outcome measure: incidence of pneumonia (a leading cause of child mortality in Afghanistan)
Findings: No benefit
VDAART (,Vitamin D Antenatal Asthma Reduction Trial) (2016, U.S.)
Participants: 881 pregnant women ages 18 to 39, determined to be at risk of having children with asthma
Intervention: 4000 IUs daily of Vitamin D versus placebo (both groups received a prenatal vitamin that contained 400 IUs of Vitamin D)
Outcome measure: asthma in the children, followed for 6 years
Findings: No benefit
Children at risk of flu (2010, Japan)
Participants: 430 children ages 3 to 15
Intervention: 1200 IUs of Vitamin D3 daily vs. placebo for four months in the winter
Outcome measure: incidence of flu (Influenza A)
Findings: Benefit: decreased incidence of flu (18.6% of children in the placebo group and 10.8% of children in Vitamin D group were diagnosed with flu)
VIDA (Vitamin D Add-on Therapy Enhances Corticosteroid Responsiveness in Asthma) Trial (2014, U.S.)
Participants: 408 Vitamin D-deficient adults with symptomatic asthma
Intervention: 100,000 IU Vitamin D once, then 4000 IU daily for 28 weeks vs. placebo (both groups received an inhaled steroid)
Outcome measure: asthma exacerbation
Findings: No benefit, but those receiving Vitamin D were able to decrease their average inhaled corticosteroid doses (unclear clinical relevance)
VIDARIS Trial (2012, New Zealand)
Participants: 322 healthy adults
Intervention: 200,000 IUs Vitamin D3 once, 200,000 one month later, then 100,000 monthly vs. placebo for 18 months
Outcome measure: upper respiratory tract infections
Findings: No benefit
,ViDiCo Trial (2015, United Kingdom)
Participants: 240 adults with COPD (chronic obstructive pulmonary disease)
Intervention: 120,000 IUs Vitamin D3 every other month vs. placebo for 1 year
Outcome measure: moderate to severe exacerbation of COPD and upper respiratory infection
Findings: Benefit for COPD exacerbations only in patients with Vitamin D levels below 20 ng/ml (50 nmol/L); no benefit for upper respiratory infections
ViDiAs Trial (2015, United Kingdom)
Participants: 250 adults with asthma
Intervention: 120,000 IUs Vitamin D3 every other month vs. placebo for 1 year
Outcome measure: asthma exacerbation and upper respiratory infection
Findings: No benefit
VITAL-DEP study (2020, U.S.)
Participants: 18,353 adults over age 50 (VITAL study participants)
Intervention: 2000 international units (IUs) of Vitamin D daily vs. placebo, for five years
Outcome measure: depression or change in mood scores
Findings: No benefit
Best-D Trial (2016, United Kingdom)
Participants: 305 adults aged 65 and older
Intervention: 4000 IUs vs. 2000 IUs Vitamin D3 vs. placebo daily for one year
Outcome measure: Vitamin D 25-OH levels
Findings: Both doses raised Vitamin D levels
A sample of clinically relevant meta-analyses, grouped by condition
Vitamin D and mortality (2019)
53 RCTs included
Outcomes: mortality
Findings: Vitamin D did not change all-cause mortality, but did reduce cancer death by 16%
Cochrane Review on Vitamin D for mortality prevention (2014)
56 RCTs included
Outcomes: mortality
Findings: Vitamin D3 (but not D2) seemed to decrease mortality in elderly adults, but further RCTs warranted
Cochrane Review of Vitamin D and cancer prevention
18 RCTS included
Outcomes: cancer diagnosis
Findings: Vitamin D did not reduce the risk of cancer
U.S. Preventive Services Task Force (2011)
19 RCTs included
Outcomes: fractures, cancer
Findings: Vitamin D and calcium prevent fractures in older adults, particularly for institutionalized elderly. No benefit regarding cancer prevention.
Cochrane Review on Vitamin D for Fracture Prevention (2014)
53 RCTs included
Outcomes: fractures
Findings: Vitamin D and calcium (but not Vitamin D alone) prevented fractures in older adults
Vitamin D in patients with asthma (2018)
8 RCTs included
Outcomes: asthma attacks requiring corticosteroids
Findings: Vitamin D supplementation reduced the number of asthma attacks requiring treatment with corticosteroids
Vitamin D in acute respiratory infection prevention (2019)
25 RCTs reviewed
Outcomes: acute respiratory tract infections
Findings: Daily or weekly (but not monthly) Vitamin D supplementation reduced the risk of respiratory infections, particularly for those with severe Vitamin D deficiency (Vitamin D under 10 ng/ml (25 nmol/l))
Vitamin D for treatment of atopic dermatitis (2019)
5 RCTs included
Outcomes: severity of dermatitis
Findings: Vitamin D at doses around 1600 IUs daily seemed to decrease the severity of dermatitis
Cochrane Review of Vitamin D for treatment of multiple sclerosis (MS)
12 RCTs included
Outcomes: relapse rate, symptom relief, immunologic response
Findings: No benefit seen
Part 1 can be read here. It addresses the basic science of what Vitamin D does on a molecular level, reviewing studies in humans, mice, and cell cultures.
Part 2 reviews the problems that can occur with high-dose Vitamin D and can be read here.
Top image by sean gladwell at bigstockphoto.com
From us to your inbox weekly.